Study: Personalized, closed-loop neuromodulation can (one day) become a “pacemaker for the brain”
Treating Severe Depression with On-Demand Brain Stimulation (UCSF press release):
UCSF Health physicians have successfully treated a patient with severe depression by tapping into the specific brain circuit involved in depressive brain patterns and resetting them using the equivalent of a pacemaker for the brain.
“This study points the way to a new paradigm that is desperately needed in psychiatry,” said Andrew Krystal, PhD, professor of psychiatry and member of the UCSF Weill Institute for Neurosciences. “We’ve developed a precision-medicine approach that has successfully managed our patient’s treatment-resistant depression by identifying and modulating the circuit in her brain that’s uniquely associated with her symptoms.”
Previous clinical trials have shown limited success for treating depression with traditional deep brain stimulation (DBS), in part because most devices can only deliver constant electrical stimulation, usually only in one area of the brain. A major challenge for the field is that depression may involve different brain areas in different people.
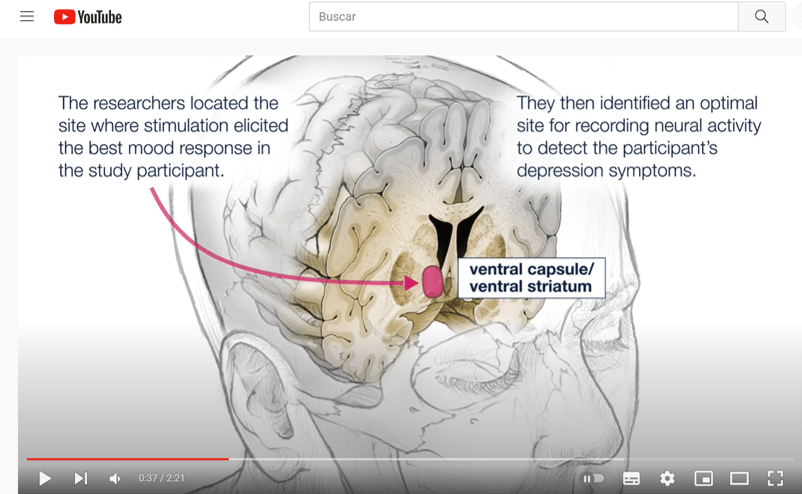
What made this proof-of-principle trial successful was the discovery of a neural biomarker – a specific pattern of brain activity that indicates the onset of symptoms – and the team’s ability to customize a new DBS device to respond only when it recognizes that pattern. The device then stimulates a different area of the brain circuit, creating on-demand, immediate therapy that is unique to both the patient’s brain and the neural circuit causing her illness.
This customized approach alleviated the patient’s depression symptoms almost immediately, Krystal said, in contrast to the four- to eight-week delay of standard treatment models and has lasted over the 15 months she has had the implanted device. For patients with long-term, treatment-resistant depression, that result could be transformative … To personalize the therapy, Chang put one of the device’s electrode leads in the brain area where the team had found the biomarker and the other lead in the region of Sarah’s depression circuit where stimulation best relieved her mood symptoms. The first lead constantly monitored activity; when it detected the biomarker, the device signaled the other lead to deliver a tiny (1mA) dose of electricity for 6 seconds, which caused the neural activity to change.
The Study:
Closed-loop neuromodulation in an individual with treatment-resistant depression (Nature Medicine)
- Abstract: Deep brain stimulation is a promising treatment for neuropsychiatric conditions such as major depression. It could be optimized by identifying neural biomarkers that trigger therapy selectively when symptom severity is elevated. We developed an approach that first used multi-day intracranial electrophysiology and focal electrical stimulation to identify a personalized symptom-specific biomarker and a treatment location where stimulation improved symptoms. We then implanted a chronic deep brain sensing and stimulation device and implemented a biomarker-driven closed-loop therapy in an individual with depression. Closed-loop therapy resulted in a rapid and sustained improvement in depression. Future work is required to determine if the results and approach of this n-of‑1 study generalize to a broader population.
The Study in Context:
- FDA clears deep transcranial magnetic stimulation device to treat obsessive-compulsive disorder
- Persistence pays off: After 8?year follow-up, study finds robust and sustained antidepressant response to deep brain stimulation (DBS)
- Machine-learning study finds EEG brain signatures that predict response to antidepressant treatments