Q: What do people with schizophrenia, bipolar disorder, depression, addiction, obsessive-compulsive disorder, and anxiety have in common? A: A brain with similar gray-matter loss
.
Different mental disorders cause same brain-matter loss, study finds (press release):
“A meta-analysis of 193 brain-imaging studies shows similar gray-matter loss in the brains of people with diagnoses as different as schizophrenia, depression and addiction…The findings call into question a longstanding tendency to distinguish psychiatric disorders chiefly by their symptoms rather than their underlying brain pathology.
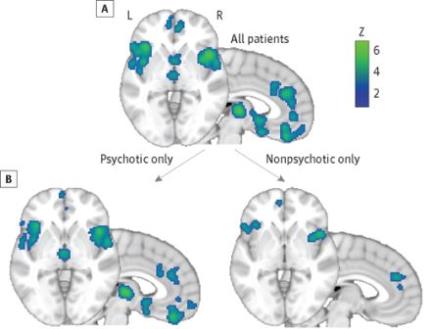
…pooled data from 193 separate studies containing, in all, magnetic-resonance images of the brains of 7,381 patients falling into six diagnostic categories: schizophrenia, bipolar disorder, major depression, addiction, obsessive-compulsive disorder and a cluster of related anxiety disorders. Comparing the images with those from 8,511 healthy control subjects, the research team identified three separate brain structures, several centimeters apart from one another, with a diminished volume of gray matter, the brain tissue that serves to process information. These structures — the left and right anterior insula and the dorsal anterior cingulate — are known to be parts of a larger network in the brain whose component parts tend to fire in synchrony. This network is associated with higher-level executive functions such as concentrating in the face of distractions, multitasking or task-switching, planning and decision-making, and inhibition of counterproductive impulses.
Gray matter loss in the three brain structures was similar across patients with different psychiatric conditions, the researchers found.”
Study: Identification of a Common Neurobiological Substrate for Mental Illness (JAMA Psychiatry)
- Importance: Psychiatric diagnoses are currently distinguished based on sets of specific symptoms. However, genetic and clinical analyses find similarities across a wide variety of diagnoses, suggesting that a common neurobiological substrate may exist across mental illness.
- Main Outcomes and Measures: We tested for areas of common gray matter volume increase or decrease across Axis I diagnoses, as well as areas differing between diagnoses. Follow-up analyses on other healthy participant data sets tested connectivity related to regions arising from the meta-analysis and the relationship of gray matter volume to cognition.
- Results: Based on the voxel-based morphometry meta-analysis of 193 studies comprising 15?892 individuals across 6 diverse diagnostic groups (schizophrenia, bipolar disorder, depression, addiction, obsessive-compulsive disorder, and anxiety), we found that gray matter loss converged across diagnoses in 3 regions: the dorsal anterior cingulate, right insula, and left insula. By contrast, there were few diagnosis-specific effects, distinguishing only schizophrenia and depression from other diagnoses…
- Conclusions and Relevance: We identified a concordance across psychiatric diagnoses in terms of integrity of an anterior insula/dorsal anterior cingulate–based network, which may relate to executive function deficits observed across diagnoses. This concordance provides an organizing model that emphasizes the importance of shared neural substrates across psychopathology, despite likely diverse etiologies, which is currently not an explicit component of psychiatric nosology.
To learn more, check out this slidedeck on the future of mental health and non-invasive neurotechnology:


