Hopes and Questions raised by Alzheimer’s drug Leqembi (lecanemab)
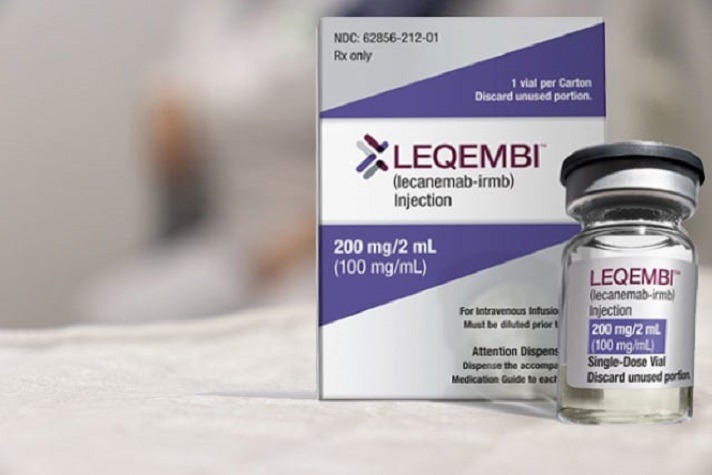 The FDA has approved Leqembi, the first disease-modifying treatment for early-stage Alzheimer’s and a precursor condition, mild cognitive impairment. Medicare has said it will pay for the therapy. Medical centers across the country are scrambling to finalize policies and procedures for providing the medication to patients, possibly by summer’s end or early autumn.
The FDA has approved Leqembi, the first disease-modifying treatment for early-stage Alzheimer’s and a precursor condition, mild cognitive impairment. Medicare has said it will pay for the therapy. Medical centers across the country are scrambling to finalize policies and procedures for providing the medication to patients, possibly by summer’s end or early autumn.
It’s a fraught moment, with hope running high for families and other promising therapies such as donanemab on the horizon. Still, medical providers are cautious. “This is an important first step in developing treatments for complex neurodegenerative diseases, but it’s just a first step,” said Ronald Petersen, director of the Mayo Clinic’s Alzheimer’s Disease Research Center in Rochester, Minnesota.
Unanswered questions abound as this new era of treatment begins for mild cognitive impairment and early-stage Alzheimer’s. Will Leqembi’s primary benefit — a slight slowing of decline in cognition and functioning — make a significant difference to patients and family members or will it be difficult to discern? Will its effects accelerate, decelerate, or flatten out over time?
Will demand for Leqembi (the brand name for lecanemab), a monoclonal antibody that requires infusions every two weeks, be robust or restrained? How many older adults in their 70s and 80s will be able and willing to travel to medical centers for infusions twice a month and have regular MRI scans and physician visits to monitor for potential side effects such as brain bleeds or swelling?
Even with Medicare coverage, how many people will be able to afford the suite of medical services required, including cognitive tests, infusions, doctors’ appointments, MRI scans, genetic tests, and spinal taps or PET scans to verify the presence of amyloid plaques, a hallmark of Alzheimer’s and a precondition for receiving this therapy?
Will primary care physicians start routinely screening older adults for mild cognitive impairment, something that doesn’t happen currently?
These questions aren’t surprising, given that these dementia treatments are opening uncharted territory. Here’s some of what people should know:
Leqembi basics. Leqembi is very effective at removing amyloid plaques (a protein that clumps between neurons) from people’s brains. But it doesn’t reverse cognitive decline or prevent future deterioration.
In a briefing document, Eisai, the company that makes Leqembi, said clinical trials showed a 27% slower rate of decline for people taking the drug. But when raw scores on the cognitive scale used to measure results are considered (4.41 for the Leqembi group at the end of 18 months versus 4.86 for the placebo group), the rate of improvement was 9%, according to Lon Schneider, a professor of psychiatry, neurology, and gerontology at the University of Southern California’s Keck School of Medicine.
Benefits may be hard to detect. Research suggests that patients notice a “clinically meaningful” change in cognitive performance — a noticeable alteration in their ability to think, remember, and perform daily tasks — when scores rise at least 1 point on an 18-point scale used to measure Leqembi’s impact. But the change detected after 18 months for patients taking this medication was only 0.45%.
“That’s a minimal difference, and people are unlikely to perceive any real alteration in cognitive functioning,” said Alberto Espay, a professor of neurology at the University of Cincinnati College of Medicine.
Petersen has a different perspective since many patients have told him they’d be happy to put off getting worse. “If we can keep these patients stable for a somewhat longer period of time, that’s meaningful,” he told me.
Side effects are common. The drugmaker reported 17% of patients taking Leqembi experienced swelling in the brain and 13% had brain bleeds. Most of these side effects occurred during the first three months of treatment and resolved without serious consequences four months later.
In slightly more than 1 in 4 cases, there were also infusion-related side effects — chills, aches, nausea, vomiting, a spike or drop in blood pressure, and more.
A little-discussed side effect is a reduction in brain volume associated with Leqembi and other anti-amyloid therapies. “We don’t know what this will mean to patients long term, and that’s concerning,” Espay said.
Because people with the APOE4 gene variant, which raises the risk of Alzheimer’s, are also at higher risk of Leqembi side effects, physicians at major medical centers will recommend genetic testing as they evaluate potential patients.
Not all patients will qualify. “I’m very carefully selecting the patients I think will be appropriate, focusing on people with mild cognitive symptoms who are otherwise healthy,” said Erik Musiek, an associate professor of neurology at the Washington University School of Medicine in St. Louis.
He has about 20 patients ready to start treatment once Washington University starts offering Leqembi, perhaps by early autumn. Delivering this therapy “is going to be challenging, and I think we need to err on the side of caution,” he said.
In Los Angeles, UCLA Health has set up a multidisciplinary group of specialists, similar to a cancer tumor board, to undertake comprehensive reviews of patients who want to take Leqembi, said Keith Vossel, director of UCLA’s Mary S. Easton Center for Alzheimer’s Research and Care. They will disqualify people with evidence of more than four microbleeds on brain MRIs, those taking blood thinners, and those with a history of seizures.
At the Mayo Clinic in Minnesota, a new Alzheimer’s therapeutics clinic will carefully assess potential patients over three to four days and treat only people who live within a 100-mile radius. “We’ll start with patients who are fairly healthy and follow them very closely,” Petersen said.
At Mount Sinai School of Medicine in New York City, Mary Sano, director of Alzheimer’s Disease Research, is concerned about older patients with mild cognitive impairment who want to take Leqembi but don’t have evidence of amyloid plaque accumulation in their brains. “We’ll only treat people who are amyloid-positive, and I’m afraid this could lead to people feeling like we’re not taking care of them,” she said. About 40% to 60% of patients 58 and older with mild cognitive impairment are amyloid-positive, research indicates.
Also of concern are patients who have moderate Alzheimer’s or early-stage cognitive impairment due to vascular dementia or various metabolic causes. They, too, would not be able to take Leqembi and may well be disappointed, Sano noted.
Costs could be considerable. Costs for Leqembi are difficult to calculate since Medicare officials haven’t announced what the government will pay for services. But the University of Southern California estimates that a year’s worth of care, including the $26,500 cost of the medication, could total about $90,000, according to Schneider.
A separate analysis by the Institute for Clinical and Economic Review suggests that all the medical services necessary to administer the drug, monitor patients, and undertake needed testing could total an average of $82,500 yearly on top of Leqembi’s direct cost.
Assuming a patient copayment of 20%, that would mean at least $18,000 in out-of-pocket spending. While many older adults have supplemental insurance (a Medigap plan or employer-sponsored retiree coverage) to cover these costs, nearly 1 in 10 Medicare beneficiaries lack this type of protection. And it remains to be seen what policies private Medicare Advantage plans will put in place for this medication.
 – Kaiser Health News contributing columnist Judith Graham focuses on medical issues and advice associated with aging and end-of-life care, helping America’s 45 million seniors and their families navigate the health care system.
– Kaiser Health News contributing columnist Judith Graham focuses on medical issues and advice associated with aging and end-of-life care, helping America’s 45 million seniors and their families navigate the health care system.


