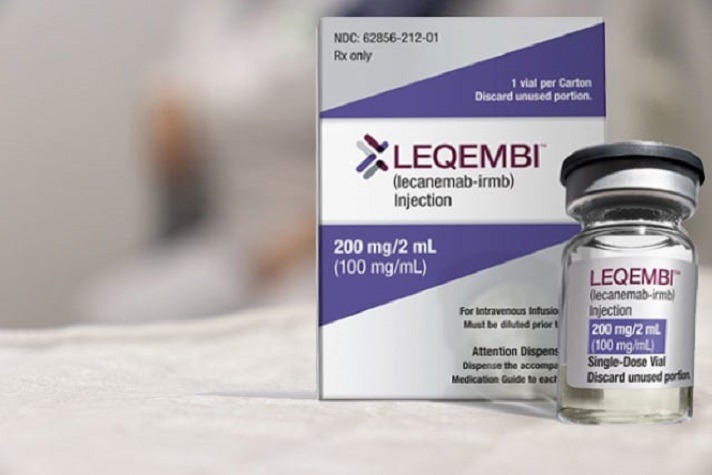
CMS: anti-amyloid drug Leqembi (lecanemab) doesn’t meet the “reasonable and necessary” standard required for wider Medicare coverage
 CMS Sticks to Sharply Limited Coverage of New Alzheimer’s Drug, Leqembi (Managed Healthcare Executive):
CMS Sticks to Sharply Limited Coverage of New Alzheimer’s Drug, Leqembi (Managed Healthcare Executive):
For now, CMS (Note: Centers for Medicare & Medicaid Services) is sticking to the coverage decision it made for Aduhelm (aducanumab) and applying it Leqembi (lecanemab). The decision limits Medicare coverage of the two Alzheimer disease’s drugs to Medicare beneficiaries who have enrolled in clinical trials of the drugs
The decision, which was announced in a press release yesterday, was denounced in strong language by the Alzheimer’s Association.
“CMS’ role is to provide health care coverage” said Joanne Pike, Dr.Ph., the organization’s president and CEO, in a prepared statement. “Their role is not to single out people living with Alzheimer’s and decide that their lives, their independence and their memories are not necessary.”
When CMS announced its “coverage with evidence development” for Aduhelm in April 2022, it said the policy would apply not just to Aduhelm but to “any future monoclonal antibodies directed against amyloid approved by the FDA with an indication for use in treating Alzheimer’s disease.” That announcement said CMS believes “important questions still need to be answered to support people with Medicare, caregivers, and their referring and treating physicians to make informed, appropriate decisions about use of any drug in this particular class” and that the data collected from having people enroll in trials “may be used to assess whether outcomes seen in carefully controlled clinical trials (e.g., FDA trials) are reproduced in the real-world and in a broader range of patients.”
The Announcement:
Response to Alzheimer’s Association’s Request to Reconsider the Final National Coverage Determination (CMS Statement):
… After careful review of the request and supporting documentation, we are making this decision because, as of the date of this letter, there is not yet evidence meeting the criteria for reconsideration. CMS’s letter to the Alzheimer’s Association outlines the key questions that need to be addressed for reconsideration. As defined in statute, to provide coverage nationally, CMS is required to examine whether a medication is reasonable and necessary. This standard differs from the criteria used by the FDA to assess whether medications are safe and effective. We are aware that additional publications may be forthcoming that include information relevant to the questions included in the current NCD. CMS will expeditiously review any new evidence that becomes available that could lead to a reconsideration and change in the NCD, such as evidence that answers the Coverage with Evidence Development (CED) questions or approval by the FDA based upon evidence of clinical benefit.
If a monoclonal antibody directed against amyloid for the treatment of Alzheimer’s disease subsequently receives traditional FDA approval, CMS will provide broader coverage using the framework we announced last year, under CED, on the same day. As noted in the NCD, coverage through CED includes registry-based studies that reflect real-world care. Registry-based studies could answer the CED questions and potentially provide greater access nationwide at more treatment sites, more rapidly, than any other coverage pathway. The CED could also help fill evidence gaps for patients who were vastly underrepresented in initial trials. CMS looks forward to discussing with patients, their families, and other stakeholders how registries could enable widespread access.


