Can COVID-19 coronavirus “invade” human brain tissue? (Quick answer: evidence so far is mixed)
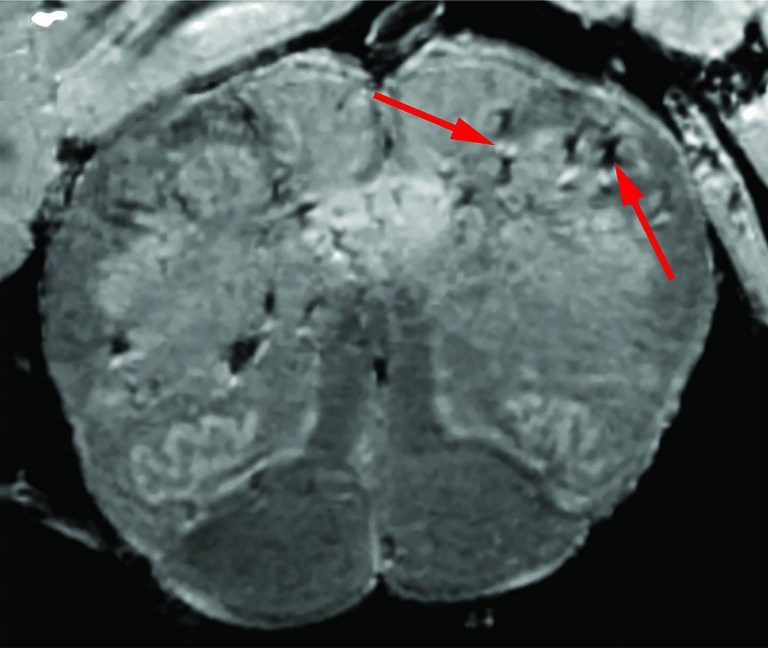
Brain scans show lower part of a COVID-19 patient’s brain stem, postmortem. Arrows point to light and dark spots suggesting blood vessel damage, without signs of infection by the coronavirus that causes COVID-19. Credit: National Institute of Neurological Disorders and Stroke, NIH
Taking a Closer Look at COVID-19’s Effects on the Brain (NIH Director’s blog):
While primarily a respiratory disease, COVID-19 can also lead to neurological problems. The first of these symptoms might be the loss of smell and taste, while some people also may later battle headaches, debilitating fatigue, and trouble thinking clearly, sometimes referred to as “brain fog.” All of these symptoms have researchers wondering how exactly the coronavirus that causes COVID-19, SARS-CoV‑2, affects the human brain.
In search of clues, researchers at NIH’s National Institute of Neurological Disorders and Stroke (NINDS) have now conducted the first in-depth examinations of human brain tissue samples from people who died after contracting COVID-19. Their findings, published in the New England Journal of Medicine, suggest that COVID-19’s many neurological symptoms are likely explained by the body’s widespread inflammatory response to infection and associated blood vessel injury—not by infection of the brain tissue itself … The team focused on the brain’s olfactory bulb that controls our ability to smell and the brainstem, which regulates breathing and heart rate. Based on earlier evidence, both areas are thought to be highly susceptible to COVID-19.
Indeed, the MRI images revealed in both regions an unusual number of bright spots, a sign of inflammation … perhaps equally noteworthy is what Nath and colleagues didn’t see in those samples. They could find no evidence in the brain tissue samples that SARS-CoV‑2 had invaded the brain tissue. In fact, several methods to detect genetic material or proteins from the virus all turned up empty.
The findings are especially intriguing because there has been some suggestion based on studies in mice that SARS-CoV‑2 might cross the blood-brain barrier and invade the brain…Another recent report in the Journal of Experimental Medicine, which used mouse and human brain tissue, suggests that SARS-CoV‑2 may indeed directly infect the central nervous system, including the brain.
The Studies:
- Microvascular Injury in the Brains of Patients with Covid-19 (New England Journal of Medicine)
- Neuroinvasion of SARS-CoV‑2 in human and mouse brain (Journal of Experimental Medicine). Abstract: Although COVID-19 is considered to be primarily a respiratory disease, SARS-CoV‑2 affects multiple organ systems including the central nervous system (CNS). Yet, there is no consensus on the consequences of CNS infections. Here, we used three independent approaches to probe the capacity of SARS-CoV‑2 to infect the brain. First, using human brain organoids, we observed clear evidence of infection with accompanying metabolic changes in infected and neighboring neurons. However, no evidence for type I interferon responses was detected. We demonstrate that neuronal infection can be prevented by blocking ACE2 with antibodies or by administering cerebrospinal fluid from a COVID-19 patient. Second, using mice overexpressing human ACE2, we demonstrate SARS-CoV‑2 neuroinvasion in vivo. Finally, in autopsies from patients who died of COVID-19, we detect SARS-CoV‑2 in cortical neurons and note pathological features associated with infection with minimal immune cell infiltrates. These results provide evidence for the neuroinvasive capacity of SARS-CoV‑2 and an unexpected consequence of direct infection of neurons by SARS-CoV‑2.
Studies in Context:
- NIH Strategic Response to COVID-19
- Survey finds ischaemic stroke and altered mental status as most common neurological complications in severe COVID-19 cases
- Neurological Implications of COVID-19 Infections
- Three ways to protect your mental health during –and after– COVID-19
- Exploring the human brain and how it responds to stress (1/3)


