The way we approach Mental Health today is broken beyond repair. The question is, what comes next, and how fast can we get there?
 The hidden links between mental disorders (Nature):
The hidden links between mental disorders (Nature):
In 2018, psychiatrist Oleguer Plana-Ripoll was wrestling with a puzzling fact about mental disorders. He knew that many individuals have multiple conditions — anxiety and depression, say, or schizophrenia and bipolar disorder. He wanted to know how common it was to have more than one diagnosis, so he got his hands on a database containing the medical details of around 5.9 million Danish citizens.
He was taken aback by what he found. Every single mental disorder predisposed the patient to every other mental disorder — no matter how distinct the symptoms. “We knew that comorbidity was important, but we didn’t expect to find associations for all pairs,” says Plana-Ripoll, who is based at Aarhus University in Denmark.
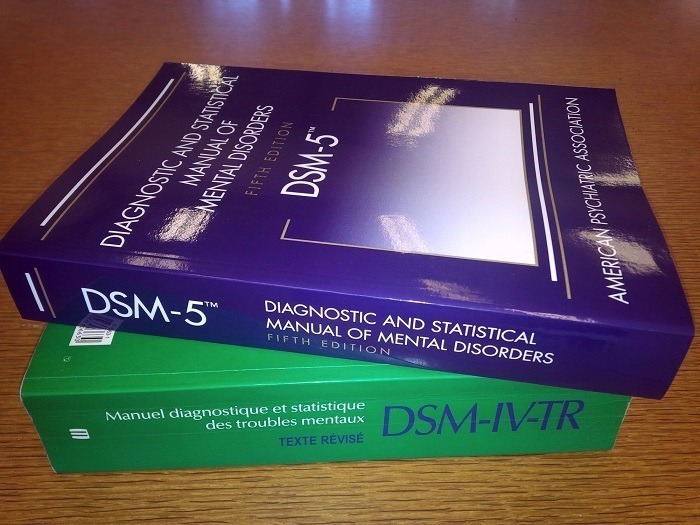
The study tackles a fundamental question that has bothered researchers for more than a century. What are the roots of mental illness? … The idea that mental illness can be classified into distinct, discrete categories such as ‘anxiety’ or ‘psychosis’ has been disproved to a large extent. Instead, disorders shade into each other, and there are no hard dividing lines — as Plana-Ripoll’s study so clearly demonstrated…
As a result, the world’s largest funder of mental-health science, the US National Institute of Mental Health, changed the way it funded research. Beginning in 2011, it began demanding more studies of the biological basis of disorders, instead of their symptoms, under a programme called the Research Domain Criteria. There has since been an explosion of research into the biological basis of psychopathology, with studies focusing on genetics and neuroanatomy, among other fields.
The Study:
Exploring Comorbidity Within Mental Disorders Among a Danish National Population (JAMA Psychiatry). Key Points from the study:
- Question: After an individual receives a diagnosis of a specific mental disorder, does the risk of developing other mental disorders increase?
- Findings: This population-based cohort study of 5 940 778 individuals, followed up for 83.9 million person-years, found that comorbidity within mental disorders was pervasive (there was an increased risk of developing all other mental disorders after an index mental disorder) and that the risk of developing comorbidity was most prominent in the first year after the onset of a mental disorder; however, the increased risk persisted over at least 15 years. For some disorders (eg, mood disorders) the absolute risks of developing specific later disorders (eg, anxiety disorders) was substantial (eg, 30%-40% over 5 years).
- Meaning: If clinicians and individuals with mental disorders had ready access to diagnosis‑, age‑, and sex-specific absolute risks of potential future comorbidity, this information could permit more tailored interventions and better education about self-management (ie, personalized medicine).
News in Context:
- The National Academy of Medicine (NAM) shares discussion paper to help empower 8 billion minds via the ethical adoption of digital mental health and neurotech
- 25 Key Resources to Improve Brain Health and Mental Health
- Large study with twins highlights the limited role of genetics in mental health and the importance of effective early interventions for ADHD
- Three ways to protect your mental health during –and after– COVID-19
- Neuroengineering meets neuroethics to address treatment-resistant depression
- We need to rethink neuroscience. And you can help us


